Introduction
In the realm of mental health and addiction treatment, the concept of dual diagnosis has gained significant attention. Dual diagnosis refers to the coexistence of a mental health disorder alongside a substance use disorder. This complex interplay can complicate treatment, making it imperative for healthcare professionals to devise personalized treatment plans that address both aspects simultaneously. In this article, we delve into the intricacies of tailoring treatment plans for individual needs in dual diagnosis, exploring various methodologies, challenges, and effective strategies that can lead to successful outcomes.
Tailoring Treatment Plans for Individual Needs in Dual Diagnosis
When addressing dual diagnosis, one size does not fit all. Each individual presents a unique set of circumstances that necessitate a customized approach. Tailoring treatment plans for individual needs involves understanding a person's specific mental health issues and substance use patterns while considering their personal history, social environment, and preferences.
Understanding Dual Diagnosis: A Comprehensive Overview
Dual diagnosis can manifest in various forms, requiring practitioners to recognize the nuances involved. The complexities arise from overlapping symptoms, which may lead to misdiagnosis or ineffective treatments if not properly addressed.
The Prevalence of Dual Diagnosis
Research indicates that approximately 50% of individuals with severe mental illnesses also struggle with substance abuse disorders. This staggering statistic underscores the need for integrated treatment approaches tailored specifically to these populations.
Common Mental Health Disorders Associated with Substance Use
- Depression: Often leads individuals to self-medicate with drugs or alcohol. Anxiety Disorders: Individuals may turn to substances as a coping mechanism. Bipolar Disorder: Substance use can exacerbate mood swings and affect overall stability. Post-Traumatic Stress Disorder (PTSD): Many seek solace in substances after traumatic experiences.
The Importance of Integrated Treatment Approaches
Integrated treatment involves simultaneous intervention for both mental health and substance use disorders. Research supports this holistic model as it addresses the root causes rather than merely treating symptoms.
Why Integrated Treatment is Essential
Improved Outcomes: Patients receiving integrated care show higher retention rates in treatment and better overall recovery outcomes. Holistic Understanding: It allows healthcare providers to analyze how each disorder impacts the other. Cost-Effectiveness: By consolidating treatment efforts, resources are used more efficiently.Initial Assessment: The Foundation of Tailored Plans
Before devising a treatment plan, an exhaustive assessment is crucial. This stage sets the groundwork for understanding individual needs.
Components of an Effective Assessment
- Clinical Interviews: Gather comprehensive histories regarding mental health and substance use. Standardized Assessments: Utilize validated tools to quantify severity levels across both disorders. Family Dynamics: Understand support systems and potential family-related stressors that could impact recovery.
Developing Individualized Treatment Plans
After a thorough assessment, developing tailored treatment plans becomes possible. These plans should be flexible and adaptable as recovery progresses.
Key Elements of Individualized Treatment Plans
Personalized Goals: Establish clear objectives based on individual aspirations. Therapeutic Modalities:- Cognitive Behavioral Therapy (CBT) Dialectical Behavior Therapy (DBT) Motivational Interviewing
- Group therapy Family involvement Peer support groups
Addressing Co-occurring Disorders Through Evidence-Based Practices
Evidence-based practices play a pivotal role in ensuring effective treatments are implemented within tailored plans.
Proven Interventions for Dual Diagnosis
Cognitive-behavioral therapy (CBT) aims at modifying detrimental thought patterns linked to both substance abuse and mental illness. Motivational interviewing (MI) enhances individuals' motivation for change by exploring ambivalence towards recovery. The utilization of medications like antidepressants or anti-anxiety medications must be carefully evaluated given their potential interaction with substances.Building Rapport with Clients: The Therapeutic Alliance
Establishing trust between therapists and clients is critical when tailoring treatment plans for dual diagnosis.
Strategies for Building Trustful Relationships
Show empathy and understanding towards clients’ struggles without judgment. Involve them actively in decision-making processes related to their own care. Maintain open communication channels throughout the treatment journey.Monitoring Progress: Adjusting Treatment as Needed
Regular evaluations are essential to ensure that individualized treatments remain effective throughout recovery.
Methods for Monitoring Progress
- Regular follow-up sessions Self-report surveys Feedback from family members or support networks
Challenges in Tailoring Treatment Plans
Despite best efforts, several challenges can arise when tailoring treatment plans for dual diagnosis patients.
Common Obstacles Faced by Practitioners
Variability in Patient Engagement: Some patients may lack motivation or engagement in their own recovery process. Stigma Surrounding Mental Health and Substance Abuse Disorders can hinder honest communication between clients and providers. Complexity of Diagnoses often leads to difficulties in identifying appropriate interventions quickly.Success Stories from Tailored Treatment Approaches
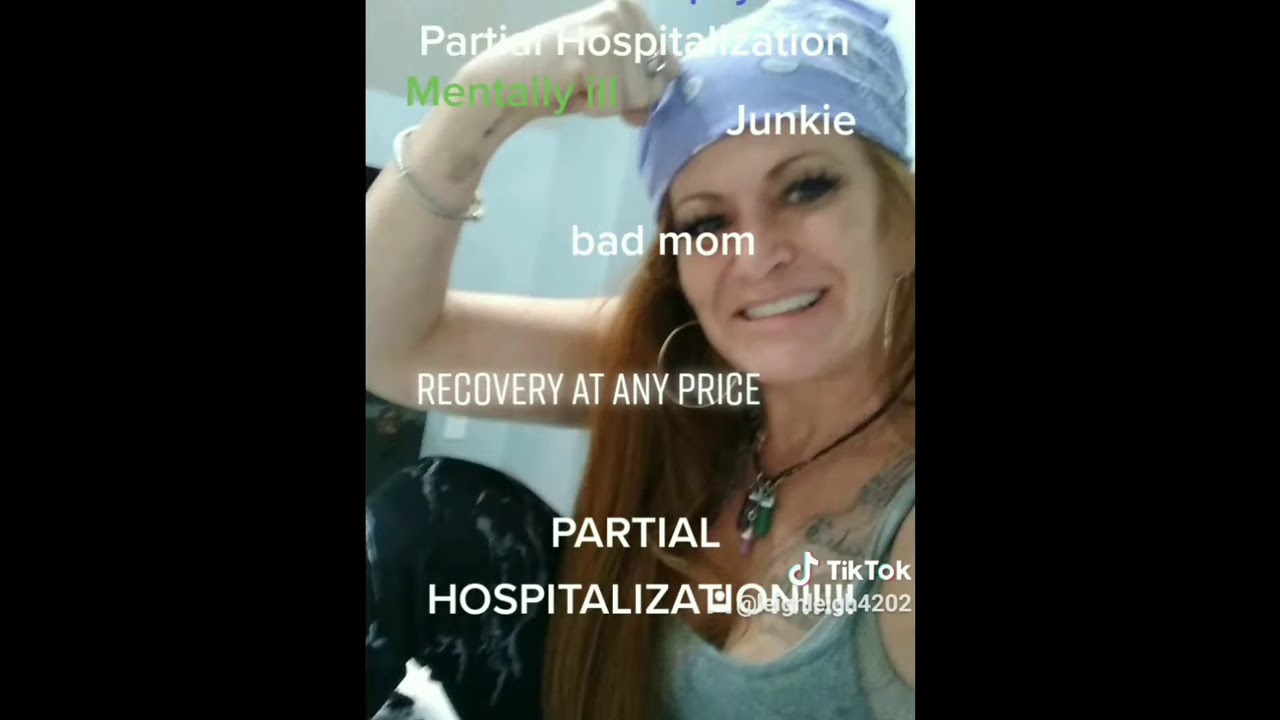
Real-life examples illustrate how effectively personalized approaches have transformed lives:
Case Study 1: Overcoming Depression through Integrated Care
A young woman diagnosed with major depressive disorder turned to alcohol as an escape during her darkest days. After entering an integrated program combining CBT techniques alongside group therapy focusing on sobriety support, she achieved remarkable progress over six months—ultimately reclaiming her life ambitions without relying on substances.
Case Study 2: Breaking Free from Bipolar Disorder
A middle-aged man grappling with bipolar disorder faced repeated relapses into drug addiction during manic episodes until he entered an intensive outpatient program emphasizing medication management combined with regular psychiatric evaluations—allowing him stability while rebuilding connections within his community confidently!
Conclusion
In conclusion, dual diagnosis requires a nuanced approach that recognizes each individual's unique circumstances while effectively addressing co-occurring mental health issues alongside substance abuse disorders through tailored treatment plans designed specifically according to their needs—a process empowered by evidence-based practices promoting positive outcomes over time!
Frequently Asked Questions (FAQs)
1. What is dual diagnosis?
Dual diagnosis refers to the co-occurrence of a mental health disorder along with a substance use disorder simultaneously affecting an individual’s wellbeing.


2. Why is it important to tailor treatment plans?
Tailoring treatment plans ensures personalized care that addresses specific needs related both mental health issues and substance misuse—leading ultimately leading toward better recovery outcomes!
3. How do I know if I have dual diagnosis?
If you find yourself struggling with both emotional difficulties (like anxiety/depression) AND using drugs/alcohol excessively—it’s recommended you seek professional help immediately!
4.What therapies work best for dual diagnosis?
Evidence-based therapies such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT) & Motivational Interviewing have shown effectiveness when treating individuals experiencing co-occurring disorders.
5.Is medication necessary in treating dual diagnoses?
While not always required; medications may be beneficial depending on individual circumstances—especially those experiencing severe symptoms impacting daily functioning!
6.Can family involvement improve outcomes?
Absolutely! Engaging family members throughout recovery creates supportive environments conducive towards long-term success—making them invaluable partners during this journey!
By employing tailored approaches within integrated frameworks emphasizing collaboration between providers/clients alike—we pave pathways https://whrcenters.com/dual-diagnosis-treatment-tampa-fl.html toward healing whilst restoring hope amidst complexities inherent within dual diagnoses!